



Rectocele, in simple terms, is defined as prolapse of the anterior rectal wall into the vagina due to weakness of the rectovaginal septum.
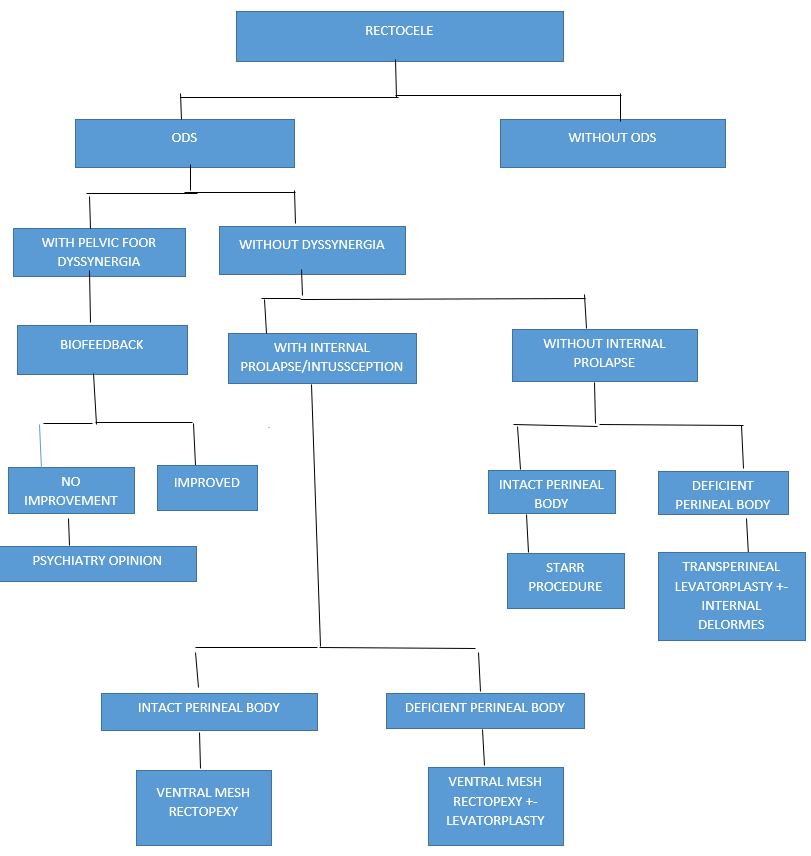
Rectoceles can occur due to chronic strain on the pelvic floor due to chronic cough or repetitive heavy lifting and worsened due to lack of hormonal support to pelvic floor. These are generally mild to moderate rectoceles and mostly require pelvic floor exercises and medical management for underlying issues. They can also occur because of chronic pelvic floor dyssynergia which will require biofeedback therapy and possible psychological workup.
The most common cause of rectoceles that require surgical intervention are those associated with injury to the pelvic floor, i.e., during vaginal birth, following surgery for anterior fistula, and trauma to the perineal body.
The most common symptoms are feeling of pelvic heaviness and pressure. Many patients start getting symptoms of obstructed defecation (ODS) and require self-digitation in the vagina or rectum to empty. When these symptoms predominate, a careful evaluation of the issue with thorough history and investigations are needed before proceeding with any intervention.
ODS in patients with rectoceles can be a “What came first: the chicken or the egg?” dilemma. As reported by Piccirilo et. al., many women with rectocele suffer from ODS, but only in the minority of them are the symptoms due to rectocele. Vermeulen et al., when reporting on the high failure rate after surgery for rectocele, stated that “to restore anatomy does not mean to restore function.”
All patients with a rectocele require a multidisciplinary evaluation with a gynecologist, colorectal surgeon, GI physiologist, psychologist, and urologist. These patients will need additional information from tests like anorectal manomety, MRI defecogram, endoanal ultrasound, and occasionally a colonic transit study.
If the history, physical examination, and diagnostic tests confirm pelvic floor dyssynergia, then without treating that by biofeedback and medications most surgical options are likely to fail.
ODS has been also defined an “iceberg syndrome”, as the two most frequent lesions, i.e., rectocele and rectal internal mucosal prolapse, present in more than 90% of patients with ODS, are easily detectable and may be considered “emerging rocks”, whereas the “surgical ship” is likely to “sink” due to the “underwater rocks”, i.e., the occult lesions. At least two occult lesions were present in all patients with ODS in a prospective study conducted by Podzemny et. al. The occult lesions include pelvic floor dyssynergia, anxiety, depression, obsessive compulsive disorder, perineal body defects, etc.
Anal manometry enables a good evaluation and diagnosis of pelvic floor dyssynergia or high-capacity rectum. MRI defecograms are good to determine grade of a rectocele and diagnose intussusception and multiorgan prolapse. Endoanal ultrasound can help evaluate sphincter and perineal body defects. Many people have additional slow transit constipation which needs to be ruled out before any surgery for rectocele.
Treatment requires a logical reasoning approach for achieving optimal results as in general the cure rates are guarded, and recurrence is high if underlying issues are not addressed. Ideally the patient – if compliant – should be evaluated by every team member, including a psychiatrist, which unfortunately in the Indian subcontinent meets with a lot of resistance. Treatment offered should consider the adverse effects. We as a rule avoid using mesh in young females because of post-operative dyspareunia and other medicolegal implications.
As a surgeon, this flow chart can be a reasonable and logical guide to approach rectocele with ODS.
Every patient is different, and the best outcomes can be achieved by a step ladder approach of conservative to surgical approach with a multidisciplinary team. The ultimate goal of the multidisciplinary team is to give the patient the best outcome with the least number of adverse effects.
REFERENCES
Piccirilo MF, Teoh TA, Yoon KS, Patino Paul RA, Lucas J, Wexner SD. Rectoceles: the incidence and clinical significante. Tech Coloproctol. 1996;2:75–79.
Podzemny V, Pescatori LC, Pescatori M. Management of Obstructed Defecation World J Gastroenterol 2015; 21 (4): 1053-1060.
Vermeulen J, Lange JF, Sikkenk AC, van der Harst E. Anterolateral rectopexy for correction of rectoceles leads to good anatomical but poor functional results. Tech Coloproctol. 2005;9:35–41.