



Primary bladder neck obstruction (PBNO) is a rare cause of voiding (and sometimes storage) LUTS in women. Literature reports an incidence of 4.6 % in middle aged women (Nitti et al 1999). PBNO can be defined as the failure of the bladder neck to open adequately during voiding, resulting in obstruction of urinary flow in the absence of anatomical obstruction, or demonstrable increased striated sphincter activity. The cause for this can be bladder neck muscle hypertrophy or abnormal muscle fiber orientation. These women typically present with slow flow of urine with sensation of incomplete void, often accompanied by straining to empty and sometimes accompanied by storage LUTS. Some patients report dull lower abdominal pain and discomfort in the urethra. Some patients may have been subjected to urethral dilatations, adding an element of iatrogenic urethral stricture to the pre-existent BNO. Late presentation may be associated with renal dysfunction.
The clinical examination usually reveals a healthy woman, sometimes with a palpable bladder and a normal vaginal examination as well as normal focused neurology. A concomitant pelvic organ prolapse must be looked for as a bladder neck kink due to large cystocoele can present with voiding LUTS.
The diagnosis needs a high index of suspicion.
Minimum evaluation after history and clinical exam must include:
The only confirmatory test is Videourodynamics (VUDS,) where simultaneous demonstration of high-pressure slow flow and non-funneling or non-relaxing bladder neck confirms the diagnosis. A separate pressure flow study and MCU can also be done if VUDS facility is not available. Though there are no widely accepted urodynamic parameters, most nomograms use Pdet at Qmax >20-25cm H20 and Qmax of <11-15ml/s as diagnostic of female BOO (Blaiwas & Groutz 2000).
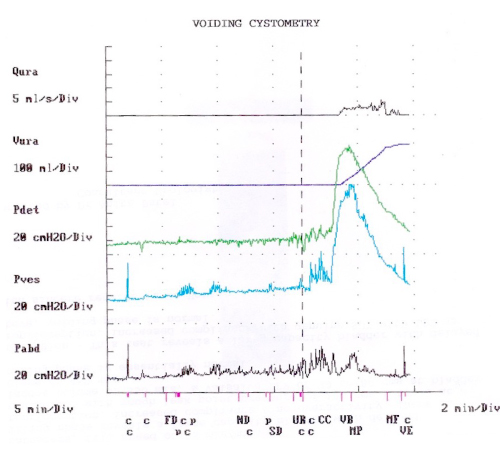
Figure 1: Typical pressure flow graph showing high pressure slow flow.
Treatment varies from observation with periodic follow-up visits and non-invasive monitoring (mild cases with minimal symptoms), to medical therapy in the form of alpha blockers such as Tamsulosin as long-term medication, to eventually surgical therapy with a bladder neck incision. Proper counseling pre-op regarding the possibility of post-op incontinence is a must. Female bladder neck incision can be performed with either bipolar diathermy or laser energy. The incisions are taken usually at 3 o’clock and 9 o’clock avoiding floor area or at 6 o’clock to prevent fistula formation (Kumar et al 1999). In some cases Clean Intermittent Catheterization may be the only practical option.
As the condition is uncommon, literature has scanty data regarding its diagnosis as well as management.
Blaivas JG, Groutz A. Bladder outlet obstruction nomogram for women with lower urinary tract symptomatology. Neurourol Urodyn. 2000;19:553–564.
Kumar A, Mandhani A, Gogoi S, Srivastava A. Management of functional bladder neck obstruction in women: use of α-blockers and pediatric resectoscope for bladder neck incision. J Urol. 1999;162:2061–2065.
Nitti VW, Tu LM, Gitlin J. Diagnosing bladder outlet obstruction in women. J Urol. 1999;161:1535–1540.
![]() The terminology documents of ICS/IUGA do not define PBNO. Do you think this complicates giving a definitive diagnosis of PBNO to women and the management? More specifically, should PBNO be recognized in international terminology documents?
The terminology documents of ICS/IUGA do not define PBNO. Do you think this complicates giving a definitive diagnosis of PBNO to women and the management? More specifically, should PBNO be recognized in international terminology documents?
![]() Yes. This is often a diagnosis of exclusion! It needs to be given identity and importance as an entity not so rare!
Yes. This is often a diagnosis of exclusion! It needs to be given identity and importance as an entity not so rare!
![]() What proportion of patients with voiding difficulty in your practice have PBNO?
What proportion of patients with voiding difficulty in your practice have PBNO?
![]() Approximately 15-20%
Approximately 15-20%
![]() What is your experience with the outcomes of bladder neck incision (BNI) for PBNO?
What is your experience with the outcomes of bladder neck incision (BNI) for PBNO?
![]() If the diagnosis is correct, the outcome is satisfactory. However, all patients should be given conservative treatment first, including medication, and should be counseled properly before offering a BNI.
If the diagnosis is correct, the outcome is satisfactory. However, all patients should be given conservative treatment first, including medication, and should be counseled properly before offering a BNI.