




Age: 75 years
Postmenopausal for 20 years
Chief Complaints:
Frequent burning micturition episodes for 4 years
Both storage and voiding LUTS (predominant storage) for 4 years
Intractable pain in urethra on passage of urine, and inability to sit
No history of foul-smelling vaginal discharge, blood in urine, flank pain, suprapubic pain, fever, episode of acute urinary retention and constipation.
Examination:
Evaluation:
Treatment History:
Cystoscopy:
Post-cystoscopy:
After 3 Weeks:
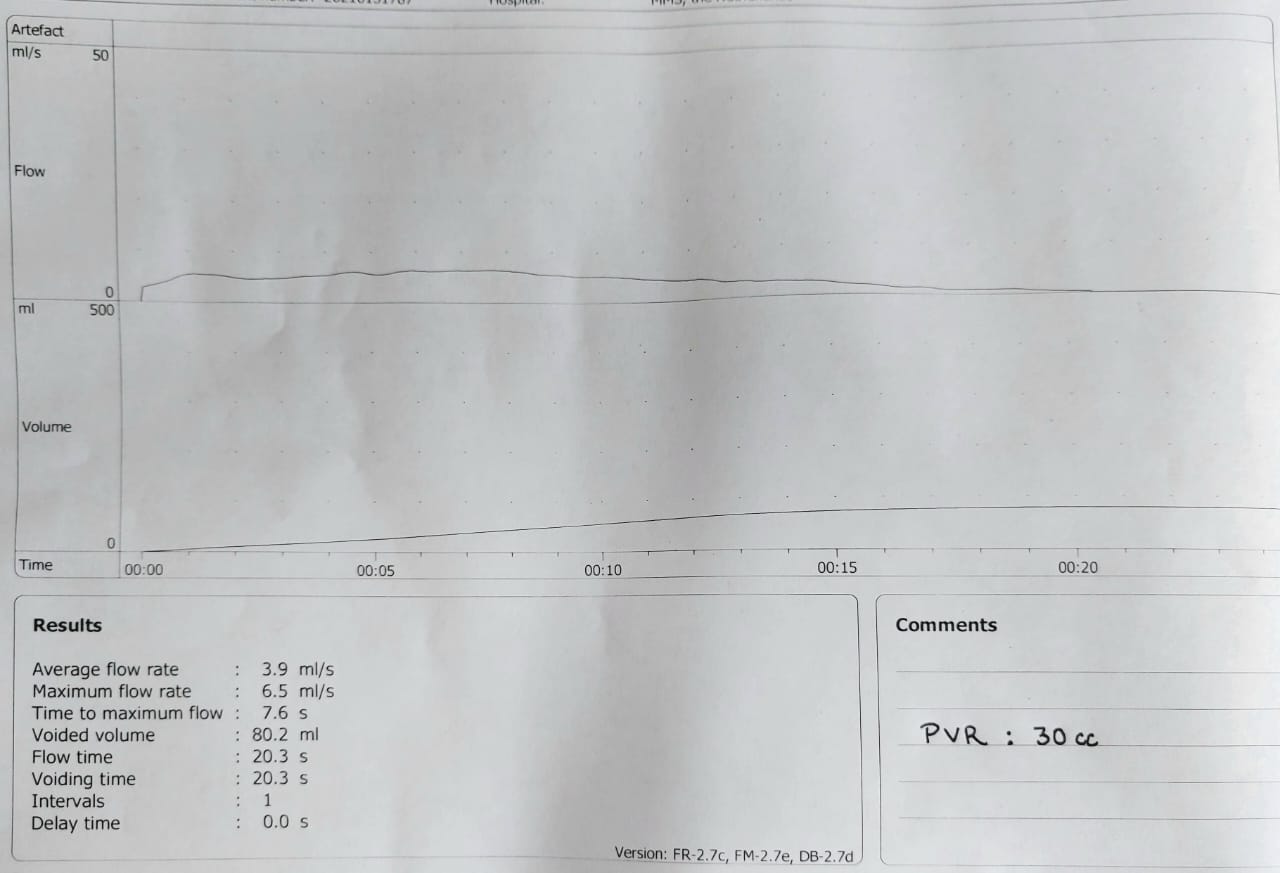
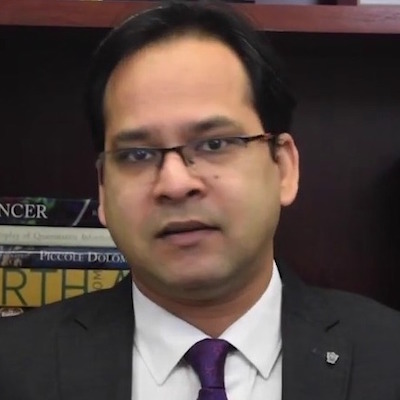
Figure 1: Uroflowmetry and post-void residual urine
Voided vol: 80.2 ml
Q max: 6.5 ml/s
Q avg: 3.9 ml/s
Voiding time :20.3 s
Flow time : 20.3 s
PVR : 30 ml
Figures 2A ,2B, 2C
Figure 2: MCU image A) right oblique B) left oblique C) anteroposterior. Red arrow shows kinking of urethra and cystocoele.

She is 75 with chief complaint being burning in urethra and pain on voiding, and clinical exam showed tenderness over urethra and atrophic changes in vagina. This is over a long time of 4 years. Urine culture showed no growth. MCUG reported ‘kinking’ in urethra on an oblique view. I noted after topical estrogen and oral antibiotics her symptoms improved 90% which is really good.
In my opinion, the urethral mucosa and rhabdosphincter are supplied with ample estrogen receptors just like the vagina (Elia 1993). The urethral mucosa as well as the sphincter can atrophy with age. Many patients with atrophy present with significant burning sensation in the urethra and the need to void frequently, leading to the symptom of frequency and often nocturnal frequency. The chronic dysuria then may lead to pelvic floor guarding (overactivity) which causes further pain and irritation maintaining this vicious cycle of pain symptoms. I noted she had pelvic floor muscle training, but this may not help as her pelvic floor actually needs relaxation rather than exercises.
I don’t think the MCUG is abnormal. The urethra is wide open during voiding and her bladder neck triangulated beautifully during voiding and you said she has no PVR. Yes, there is a bit of a curve, but it is an oblique view, and the cystocele may have distorted it a little. It is definitely not the appearance of obstruction like with a tight sling or detrusor-external sphincter dyssynergia (DESD), and there is no proximal dilation. So, I would not worry about the so-called ‘kinking’ on the radiology report. It is not obstructed and none of her history and findings support obstruction.
In summary, I think it is not the antibiotics that cured her, it is the use of topical estrogen as I mentioned above. A continence nurse should counsel her regarding bladder training to regain a better functional capacity, etc. One caveat is you reported cord-like urethra. I am not sure what you mean. A pelvic MRI may exclude unusual pathology there and if anything is suspicious, you can always refer to a urology colleague for an opinion. I recommend keeping her on estrogen for a while and get her to see a continence nurse advisor. As a multidisciplinary field, allied health advice and support is always just around the corner.
Elia G, Bergman A. Estrogen effects on the urethra: beneficial effects in women with genuine stress incontinence. Obstetrical & Gynecological Survey. July 1993:48(7):509-517.

I would remove the catheter and continue her on low dose antibiotics for the moment. I would also continue the vaginal estrogen cream. It is hard to know what to make of the “kinked” urethra. Typically, stage one anterior vaginal wall prolapse will not impact voiding to a large degree. However, on the MCU it appears the prolapse may be more significant. One option would be to reexamine her perhaps in more of a standing position and possibly offer her a pessary trial and see if her symptoms continue to improve – off the low dose antibiotics. If they do, you could then consider an operative repair or maintain the pessary. If not, restart the low dose antibiotics and consider a pelvic MRI to make sure there is not a urethral diverticulum that did not show up on MCU.