




The use of ultrasound imaging in women’s health is traditionally associated with obstetric practice and is indeed a familiar and expected part of routine follow up to both obstetricians and pregnant women alike. Due to increasing complexities of pelvic floor dysfunction, reliance on clinical assessment alone is often insufficient and this has led to the development of ultrasound imaging to aid diagnosis and guide further management of patients with a range of pelvic floor disorders.
Endo Anal Ultrasound (EAUSS) is widely used in the UK in larger centers and is indicated in the follow up of women with Obstetric Anal Sphincter Injuries (OASI) and has a role to play in the work up of patients with fecal incontinence under the colorectal surgeons; here historical occult OASI is the common cause of fecal incontinence in females. This article covers the role of EAUSS in the management of OASI, techniques in performing an EAUSS, and interpretation of the result.
OASI are defined as perineal injuries sustained during childbirth affecting the anal sphincter complex and are categorized as 3A, 3B, 3C and 4th degree tears according to the Sultan Classification (Sultan 1999), depending on the extent of involvement of the External Anal Sphincter (EAS), Internal Anal Sphincter (IAS) and rectum as described in Table 1.
Table 1
|
Degree of Tear |
Definition |
|
3A |
Involves <50% of EAS |
|
3B |
Involves >50% of EAS |
|
3C |
Involves EAS and IAS |
|
4th |
Involves both EAS, IAS and rectal mucosa |
OASI rates in the UK and abroad are increasing (Gurol-Urganci et al 2013). Between 2000 and 2012, the OASI rate in England alone tripled (Gurol-Urganci et al 2013), making it an increasingly relevant issue. Between 20-40% (Fitzpatrick et al 2000) of women will report symptoms of Anal Incontinence (AI) despite identification and repair of OASI, therefore, follow up is crucial to identify and manage these women. Asymptomatic women are an important group of women who can be overlooked in the follow up period and may too be at risk of AI in later life due to an inadequate OASI repair, further supporting the need for careful follow up of all women with OASI irrespective of symptoms.
EAUSS is the gold standard in the follow up of women with OASI. It is recommended by the Royal College of Obstetricians and Gynaecologists (RCOG) (Sultan 1999) together with anal manometry in the follow up of all women with OASI, ideally within a dedicated perineal clinic 6-12 weeks postpartum.
EAUSS allows identification of the integrity of the anal sphincter complex through identification of defects, or gaps, in the anal sphincter muscles where an OASI has been missed, identified incorrectly, or inadequately repaired. Identification of defect(s) on EAUSS can be used alongside reported symptoms and the results of anal manometry (which asses the function of the sphincter complex) to guide decision making for any potential future deliveries, allowing the option to avoid vaginal delivery altogether in favor of an elective cesarean section to avoid further compromising the sphincter complex.
Although EAUSS requires specialist equipment and training to perform and interpret the image, it is also a quick, inexpensive, and accessible bedside examination that can produce extremely useful results that benefit both the patient and the unit. Results of EAUSS can be an objective means to audit staff performance on OASI repairs and help identify staff requiring additional training as well as for research activity within the unit.
Women should ideally be followed up in a dedicated perineal clinic. This clinic should provide an adequate and convenient environment for recently delivered mothers; this would include a private place to breastfeed and areas spacious enough to accommodate prams (Fowler et al 2011).
Women should be informed of what to expect during the assessment and consent should be sought. A private space to undress and use the toilet should be provided. Women should be adequately exposed while respecting their dignity. A hospital gown should be worn, and the women should be exposed from the waist down.
The patient should be positioned in the left lateral position with knees drawn towards the chest. The EAUSS probe should be well lubricated with ultrasound gel and introduced into the anus and rectum gently and gradually.
Images are taken in the axial plane, however, newer ultrasound machines allow for 3D images to be taken and analyzed in the sagittal and coronal planes.
Once in the upper anal canal, a horseshoe structure, much like a sling, can be identified. This is the puborectalis muscle, as illustrated in Image 1.
Image 1
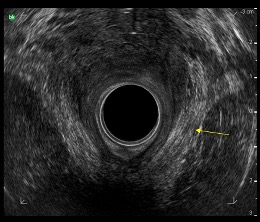
Puborectalis muscle indicated by the yellow arrow
Image courtesy of University Hospital of North Midlands Royal Stoke Hospital, Pelvic floor Clinic.
The lower regions of the anal canal can be visualized by either gradually withdrawing the probe from the rectum or using the down button feature on the probe to capture images in the lower anal canal.
In the mid region of the anal canal, the EAS and IAS can be identified. The EAS is identified as a hyper echogenic, thick, circular structure on the outermost aspect of the screen. The IAS is the hypo echogenic, black, inner ring as illustrated in Image 2. The lowest region of the anal canal will bring to view the internal anal sphincter and is immediately caudal to where it then terminates and then comprises only a subcutaneous area of the EAS.
Image 2
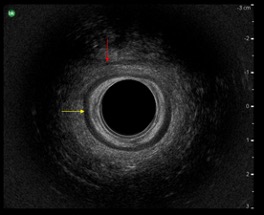
EAS indicated by red arrow; IAS indicated by the yellow arrow
Image courtesy of University Hospital of North Midlands Royal Stoke Hospital, Pelvic floor Clinic.
Images of the sphincter complex should be taken and printed to then be stored with the patient’s case notes for future reference.
Results of EAUSS are prone to subjective interpretation and are operator-dependent, highlighting the importance of adequate training in image interpretation. The image should be analyzed systematically, focusing first on identifying defects in the EAS before moving on to the IAS. Care should be taken to avoid misclassification of scars as defects to avoid over diagnosis of OASI and vice versa to avoid missing defects.
Defects are identified as disruptions or gaps in the striated muscle of the EAS and are gaps which exceed 1 hour on the clock face or >30 degrees angle (Thakar & Sultan 2003) as shown in Image 3.
Image 3
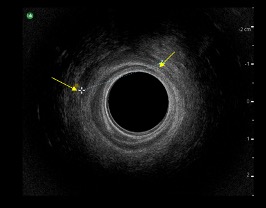
EAS defect indicated by the yellow arrows
Image courtesy of University Hospital of North Midlands Royal Stoke Hospital, Pelvic floor Clinic.
Defects in the IAS are more evident, as the IAS will no longer be visualized as a black circular structure as described in Image 4.
Image 4
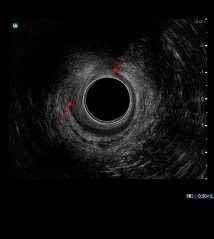
IAS defect indicated by red arrows
Image courtesy of University Hospital of North Midlands Royal Stoke Hospital, Pelvic floor Clinic.
Any defects should be documented according to its location in the anal canal, and this is across 3 cross sectional levels according to the Liverpool Pictoral Chart (LPC) of High, Mid, and Low (Thakar & Sultan 2003). An alternative method of documentation is to analyze the image across 4 levels: levels 1,2,3 and 4 as supported by the Sultan group in Croydon (Sultan 1999).
As highlighted previously, women who have sustained OASI should be followed up in a perineal clinic. This will allow optimal care to be offered from a range of skilled and experienced professionals including urogynecologists, colorectal surgeons, specialist nurses and midwives, physiotherapists, and psychosexual counselors. This care is essential for the physical and emotional healing of women following OASI.
The results of EAUSS should not be used in isolation to guide management of women with OASI but should be used alongside symptoms ascertained using validated Quality of Life (QOL) questionnaires; this includes bladder, bowel, and sexual function together with the results of Anal Manometry (AM). Patient informed choice is the single most important determinant of future mode of delivery.
Management of women based on symptoms and investigations differs from center to center, however, most would offer asymptomatic women with normal EAUSS and AM results a vaginal delivery and asymptomatic women with abnormal EAUSS or AM an elective cesarean section. Symptomatic women in general would be offered an elective cesarean section irrespective of EAUSS and AM to prevent further sphincter and pelvic floor compromise. These women would be managed conservatively with dietary advice, supervised pelvic floor therapy with biofeedback, and pharmacologically with constipating agents. Women with severe symptoms of anal incontinence, including fecal incontinence, require an individualized management plan. Women who have not completed their families would be counseled about the option of having a vaginal delivery followed by a secondary sphincter repair once their family is complete. As with all follow up of women under a perineal clinic, this would be in consultation with a multi-disciplinary team including colorectal surgeons.
As explored here, EAUSS plays a significant role in the work up of women following OASI and allows identification of sphincter defects that would be missed on clinical assessment alone, allows specialized care to be offered to women who are identified as having a sphincter defect which can improve their current symptoms and importantly can allow forward planning for future modes of delivery to prevent further injury to the sphincter complex.
Fitzpatrick M, Behan M, O’Connell PR, O’Herlihy C. A randomized clinical trial comparing primary overlap with approximation repair of third-degree obstetric tears. Am J Obstet Gynecol. 2000;183:1220–4.
Fowler G, Williams A, Murphy G, Taylor K, Wood C, Adam E. How to set up a perineal clinic. The Obstetrician and Gynaecologist. 2011;11:129-132.
Gurol-Urganci I, Cromwell DA, Edozien LC, Mahmood TA, Adams EJ, Richmond DH, et al. Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: time trends and risk factors. BJOG. 2013;120:1516–25.
Sultan AH. Obstetric perineal injury and anal incontinence. Clin Risk. 1999;5:193–6.
Thakar R, Sultan AH. Management of Obstetric Anal Sphincter Injuries. The Obstetrician and Gynaecologist 2003;5:72-8.