



Masayoshi Nomura, Auran Rosanne B. Cortes, Tokumasa Hayashi, Yugo Sawada, Shino Tokiwa, Mika Nagae, Myat Noe Swe, Kojiro Nishio, Yasutoshi Yoshimura, Ippei Oiwa, Nao Muta
Urogynecology Center, Kameda Medical Center, Kamogawa, Chiba, Japan
Sacrocolpopexy is considered the gold standard for the treatment of vaginal vault prolapse (VVP). At present, there are no universally accepted guidelines and consistent surgical technique of sacrocolpopexy.1 – 3 Since it remains as the most successful and durable surgery for the repair of apical and advanced pelvic organ prolapse (POP), it is increasingly considered as the first-line surgical option for multicompartment and advanced POP.1 – 5 Here in Japan, laparoscopic sacrocolpopexy (LSC) is indicated for VVP, multicompartment POP, symptomatic POP, and recurrent POP. In our institution, we dissect the vaginal wall extensively, i.e., full- length dissection for mesh fixation, to lower the chances of reoperation due to POP recurrence.
The main surgical steps of LSC can be divided into the following steps: dissection of the vesicovaginal and rectovaginal spaces, vaginal fixation of the mesh, and fixation of the mesh to the promontory.
Before proceeding to the main surgical steps of LSC, adequate exposure and visualization of the pelvic organs and sacral promontory area must be achieved by fixing the sigmoid colon by appendix epiploicas transparietally after mobilization. Identification of aortic bifurcation, common and internal iliac vessels, middle sacral vessels, and right ureter is essential prior to peritoneal incision, so that these structures can be avoided. The accurate position of L5-S1 is confirmed by tactile feedback, and the peritoneum is incised over the bony prominence and extended along the white line of Toldt to meet the incision on the peritoneum that opens into the rectovaginal space.
Performing LSC for VVP poses a challenge during dissection because post-hysterectomy adhesions make the exposure of the anterior and posterior vaginal walls difficult. A full understanding on the principle of adhesiolysis, recognition of pelvic organs (bladder, rectum, vagina), and identification of the vaginal plane are necessary to perform a good dissection.
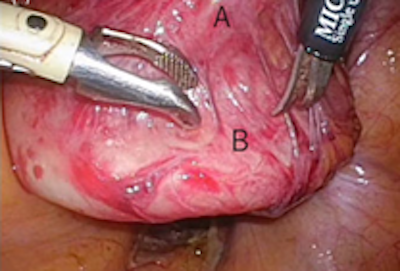
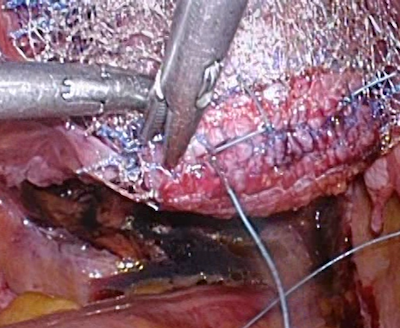
We have devised the following techniques to facilitate good dissection of the vesicovaginal space. During dissection of the vesicovaginal space, a spatula is placed in the vagina to identify the proximal extent of the apical vault. This is followed by incision of peritoneal reflection over the bladder at the junction of the vaginal vault (Figure 1a). The spatula is then removed and stay sutures are placed bilaterally at the margin of the peritoneal reflection at the vaginal vault and mesorectal fat (Figure 1b). This peritoneal fixation contributes to the creation of appropriate tension along the dissection plane and to the exposure of the proximal extent of the vaginal wall. Temporary suspension of the bladder to the abdominal wall is also effective in creating appropriate tension.
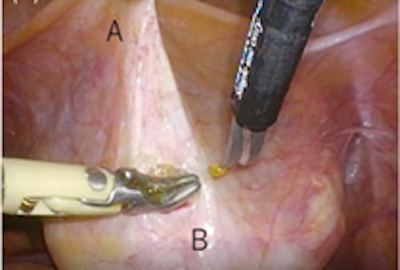
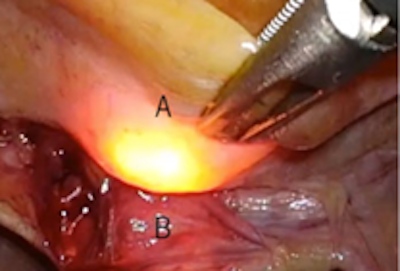
Recognition of the border between the bladder and the anterior vaginal wall is mandatory for smooth dissection of the vesicovaginal space. In cases where identification of the borders of the bladder and anterior vaginal wall is difficult, we find it helpful to use the cystoscope. The cystoscope is inserted into the urethra and passed into the bladder to recognize the extent of the border of the bladder (Figure 1c). It is also inserted into the vagina to determine the extent of the border of the anterior vaginal wall (Figure 1d). A combination of sharp and blunt dissection of the bladder away from the anterior vaginal wall along the vesicovaginal septum using scissors and forceps, respectively, is then performed as low and as close to the level of bladder neck (Figure 1e).
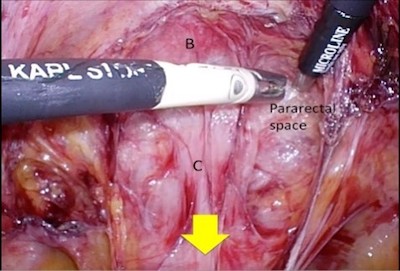
The same principle on recognition and creation of appropriate tension applies to the dissection along the rectovaginal plane. Recognition of the border between the rectum and the posterior vaginal wall is mandatory as well. A sizer can be placed into the rectum to help identify the border between the rectum and the posterior vaginal wall. Creation of appropriate tension along the dissection plane is achieved by temporary suspension of the vaginal vault to the abdominal wall and pulling the peritoneum over the rectum cranially. Dissection of the rectum away from the posterior vaginal wall involves making a window along the plane of rectovaginal septum and is extended to the level of the perineal body and lateral to the rectum to expose the levator ani muscles (Figure 1f).
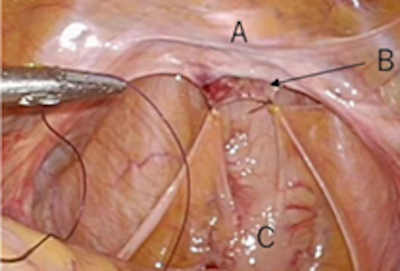
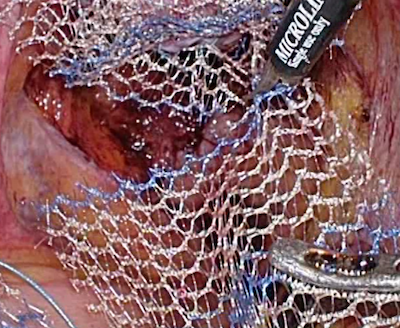
Adequate exposure of the bladder, vaginal walls, rectum, and levator ani muscles facilitates optimal positioning of the mesh. Two separate pieces of self-cut polypropylene mesh are used for fixation. The posterior mesh is anchored to levator ani muscles bilaterally with 2-0 polyester suture. Fixation of the posterior mesh should be tension-free, acting as a hammock for the posterior vaginal wall, to avoid bowel obstruction, dyspareunia, and mesh erosion. Additional anchors are placed at the bulbocavernosus bilaterally and at the most distal end of the posterior vaginal wall, at the level of perineal body using 3-0 polyester suture (Figures 2a and 2b). This is achieved by intravaginal examination of the bilateral bulbocavernosus by the surgeon while simultaneously anchoring additional sutures.
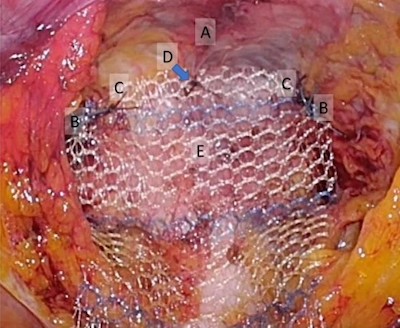
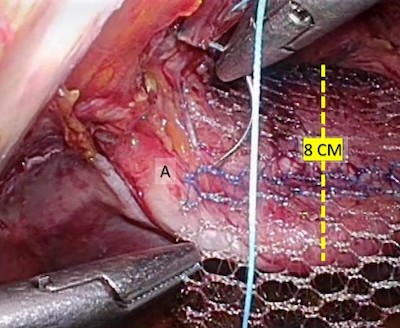
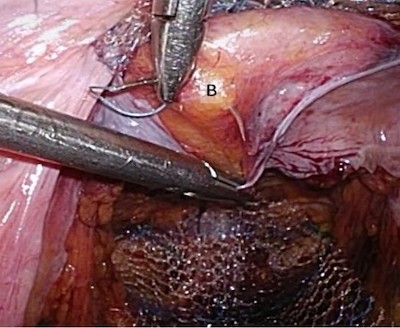
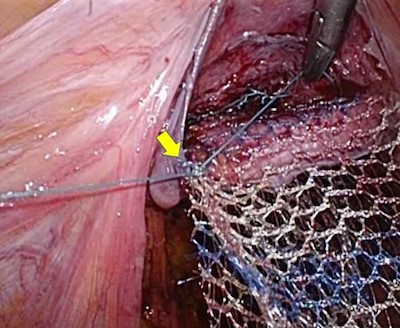
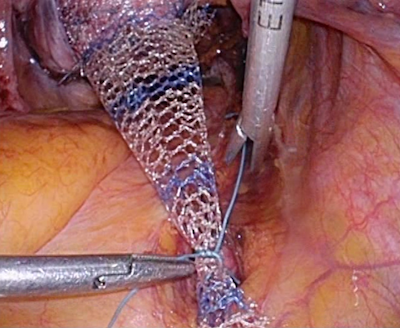
Another piece of mesh is fixed to the anterior vaginal wall. Initial anchors are placed at the distal end of the anterior vaginal wall using 3-0 polyester suture. After placement of the initial anchor sutures, a spatula is inserted into the vagina to achieve a length of 8 cm. The anterior and posterior meshes are then sutured together at the lateral edge of the vaginal vault (Figures 3a – 3c).
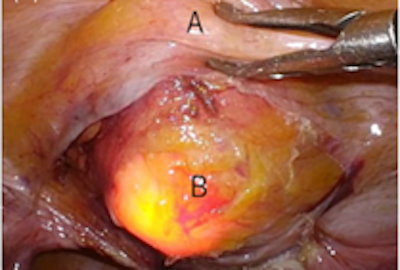
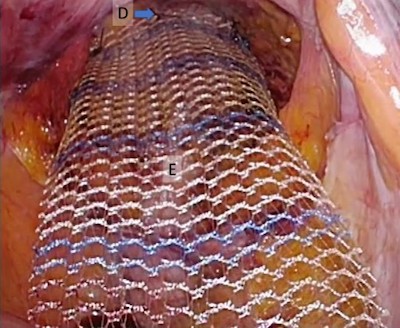
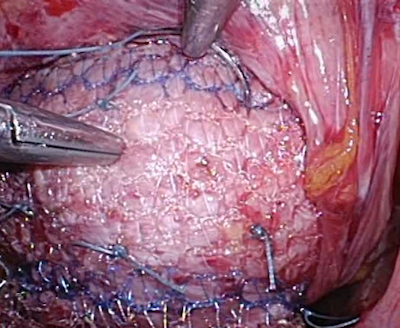
Additional sutures (7 to 10) are then placed to the anterior vaginal wall to obtain a solid attachment of the mesh. Excess posterior mesh is trimmed after anchoring it to the proximal posterior wall of the vaginal vault using 3-0 polyester suture (Figures 4a – 4c).
Care must be taken when placing the sutures to the vagina. Suture depth must be controlled to at most 2 mm depth to make sure that it is only placed through the fibromuscular layer and not into the vaginal epithelium. In relation to this, fixating the mesh to the levator ani muscles minimizes placement of sutures to the vaginal walls. Also, the posterior vaginal wall is generally thinner compared to anterior vaginal wall.7, 8
The cranial end of the anterior mesh is fixed to anterior longitudinal ligament of the L5 disc or sacral promontory with 1-0 polyester suture after appropriate level of vaginal elevation and gentle tension without undue traction on the vagina had been confirmed by vaginal examination (Figure 5). It is important to avoid placing the suture between L5-S1 disc to prevent discitis.
To date, there is no universal recommendation on what objective parameters to employ in adjusting mesh tension to determine the appropriate level of vaginal elevation. In our patients, a vaginal length of 7.5 to 8 cm is enough in creating an appropriate level of vaginal elevation and mesh tension as confirmed by vaginal examination. A study by Nomura et al. presented the use of cystoscopy to allow the visualization of the bladder wall during mesh adjustment to avoid the “central road” finding and bladder neck opening. These findings, in turn, could predispose the patients to develop de novo stress urinary incontinence (SUI). Since the study only involved a small number of cases with short follow-up period, they have mentioned that further investigation is needed to determine whether the use of cystoscopy promotes effective POP repair and de novo SUI reduction.9
We recommend closure of the peritoneum, ensuring that no mesh is left exposed, at the completion of sacrocolpopexy.
As pelvic floor surgeons, we always aim to achieve the best surgical outcome for our patients. In line with this, we would like to emphasize that a good dissection technique is one of the keys in achieving a good surgical outcome. It is imperative to be able to perform a good and safe dissection during surgery to reduce the risk of or even prevent complications such as organ injury and hemorrhage. To be able to perform a good and safe dissection, apt anatomical recognition is necessary. Easier anatomical recognition during surgery can be achieved by applying appropriate tension to expose the surgical plane of dissection.
Conflict of Interest. None declared.