Difficulty voiding in neurologically intact women can occur because of the inability of the bladder muscle to contract efficiently – detrusor underactivity (DU) or because of some blockage of the urethra – bladder outflow obstruction (BOO). BOO can be due to anatomic causes or “functional” obstruction.” Lower urinary tract symptoms due to primary detrusor underactivity are typically observed in older women, whereas functional BOO is much more likely to affect younger women.
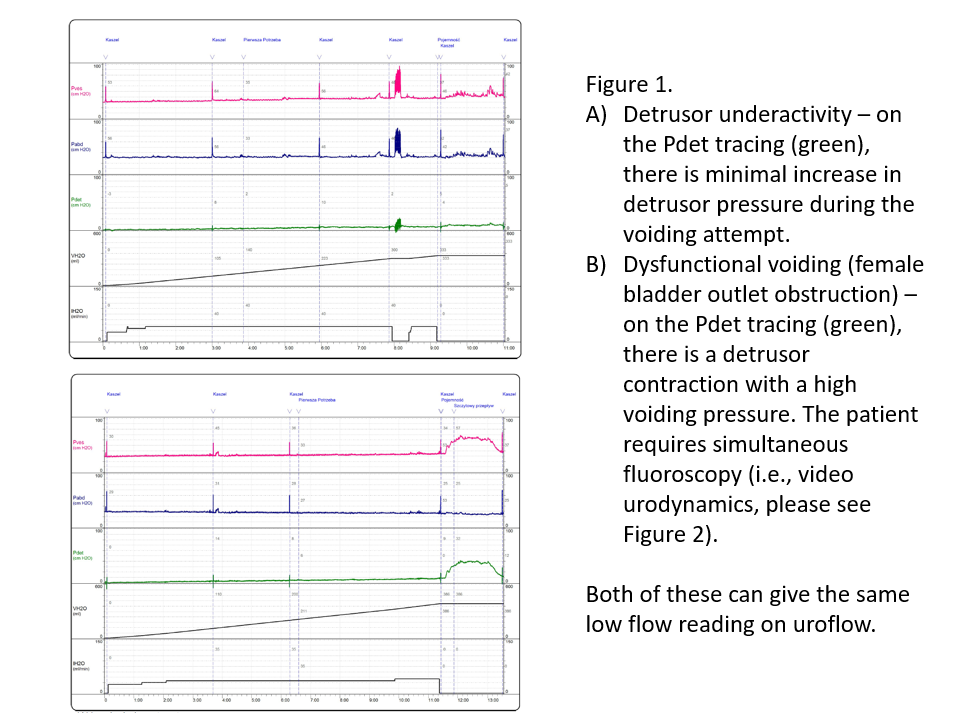
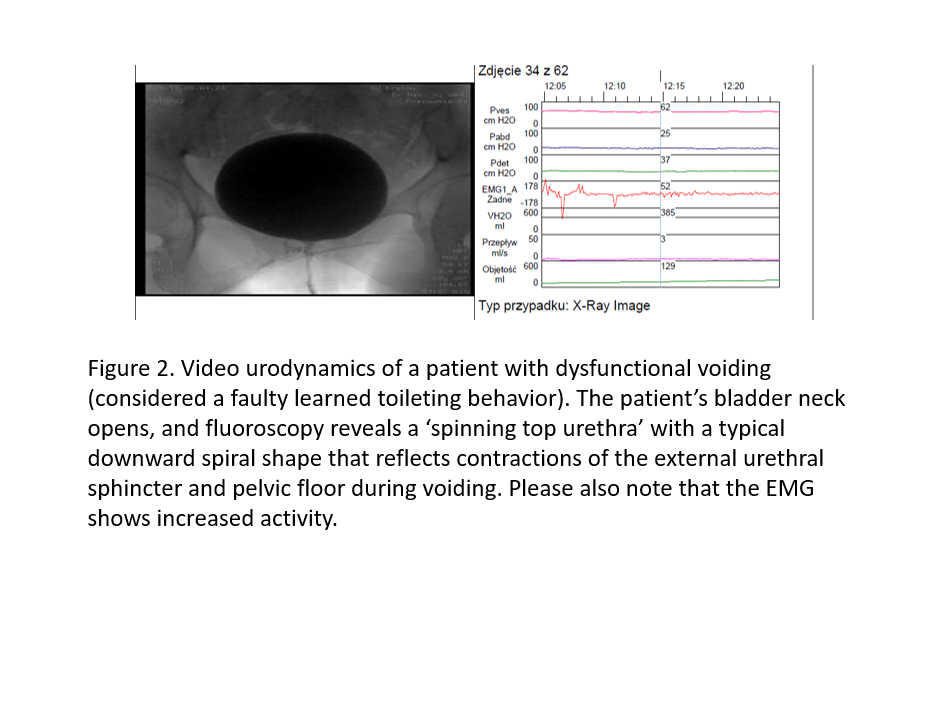
When comparing DU to dyssynergic/dysfunctional voiding (one type of functional BOO), history and physical examination will fail to differentiate between them and a multichannel urodynamic study that includes a pressure–flow analysis remains the mainstay of diagnosis. Furthermore, when evaluating patients who may have functional BOO, current guidelines recommend that urodynamics be combined with imaging to precisely delineate the level of obstruction. This refers to a videourodynamic study, but in modern literature, because of improvements in portable computing, mobile C-arm X-ray machines, and digital signal processing, the study is often termed a fluorourodynamics. The first step to differentiate these two diagnoses is to determine if there is DU or BOO. For DU, the characteristic UDS findings are a combination of low flow and concomitant low detrusor pressure, whereas, for BOO, a combination of low flow and concomitant high detrusor pressure is observed.
Dyssynergic/dysfunctional voiding is considered a learned behaviour and defined as an intermittent and/or fluctuating flow rate due to involuntary intermittent contractions of the external urethral sphincter and/or levator muscles during voiding in neurologically normal women. With concomitant imaging during a video urodynamic study, urodynamics observes a narrowing at the level of the external urethral sphincter with dilatation of the proximal urethra (‘spinning top urethra’) or intermittent contractions of the external urethral sphincter and pelvic floor during voiding in these patients.
Although both conditions may require self-catheterization, those with dysfunctional voiding often have a better prognosis, as studies demonstrate that pelvic floor physiotherapy, biofeedback, pharmacologic therapy, or sacral neuromodulation may be effective treatments for dysfunctional voiding. Select patients with DU may also respond to sacral neuromodulation.