Abstract
Introduction and hypothesis
We aimed to systematically review the literature on pelvic organ prolapse (POP) surgery with uterine preservation (hysteropexy). We hypothesized that different hysteropexy surgeries would have similar POP outcomes but varying adverse event (AE) rates.
Methods
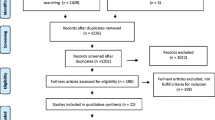
MEDLINE, Cochrane, and clinicaltrials.gov databases were reviewed from inception to January 2018 for comparative (any size) and single-arm studies (n ≥ 50) involving hysteropexy. Studies were extracted for participant characteristics, interventions, comparators, outcomes, and AEs and assessed for methodological quality.
Results
We identified 99 eligible studies: 53 comparing hysteropexy to POP surgery with hysterectomy, 42 single-arm studies on hysteropexy, and four studies comparing stage ≥2 hysteropexy types. Data on POP outcomes were heterogeneous and usually from <3 years of follow-up. Repeat surgery prevalence for POP after hysteropexy varied widely (0–29%) but was similar among hysteropexy types. When comparing sacrohysteropexy routes, the laparoscopic approach had lower recurrent prolapse symptoms [odds ratio (OR) 0.18, 95% confidence interval (CI) 0.07–0.46), urinary retention (OR 0.05, 95% CI 0.003–0.83), and blood loss (difference −104 ml, 95% CI −145 to −63 ml) than open sacrohysteropexy. Laparoscopic sacrohysteropexy had longer operative times than vaginal mesh hysteropexy (difference 119 min, 95% CI 102–136 min). Most commonly reported AEs included mesh exposure (0–39%), urinary retention (0–80%), and sexual dysfunction (0–48%).
Conclusions
Hysteropexies have a wide range of POP recurrence and AEs; little data exist directly comparing different hysteropexy types. Therefore, for women choosing uterine preservation, surgeons should counsel them on outcomes and risks particular to the specific hysteropexy type planned.

Similar content being viewed by others
References
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6. https://doi.org/10.1097/AOG.0000000000000286.
Dieter AA, Wilkins MF, Wu JM. Epidemiological trends and future care needs for pelvic floor disorders. Curr Opin Obstet Gynecol. 2015;27(5):380–4. https://doi.org/10.1097/GCO.0000000000000200.
Sisco M, Kyrillos AM, Lapin BR, Wang CE, Yao KA. Trends and variation in the use of nipple-sparing mastectomy for breast cancer in the United States. Breast Cancer Res Treat. 2016;160(1):111–20. https://doi.org/10.1007/s10549-016-3975-9.
Madsen AM, Raker C, Sung VW. Trends in Hysteropexy and apical support for Uterovaginal prolapse in the United States from 2002 to 2012. Female Pelvic Med Reconstr Surg. 2017;23(6):365–71. https://doi.org/10.1097/SPV.0000000000000426.
Korbly NB, Kassis NC, Good MM, Richardson ML, Book NM, Yip S, et al. Patient preferences for uterine preservation and hysterectomy in women with pelvic organ prolapse. Am J Obstet Gynecol. 2013;209(5):470.e471–6. https://doi.org/10.1016/j.ajog.2013.08.003.
Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2013;24(11):1803–13. https://doi.org/10.1007/s00192-013-2171-2.
Ridgeway B, Frick AC, Walter MD. Hysteropexy. A review Minerva Ginecol. 2008;60(6):509–28.
Meriwether KV, Antosh DD, Olivera CK, Kim-Fine S, Balk EM, Murphy M, et al. Uterine preservation vs hysterectomy in pelvic organ prolapse surgery: a systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol. 2018;219(2):129–46 e122. https://doi.org/10.1016/j.ajog.2018.01.018.
Wallace BC, Trikalinos TA, Lau J, Brodley C, Schmid CH. Semi-automated screening of biomedical citations for systematic reviews. BMC Bioinformatics. 2010;11:55. https://doi.org/10.1186/1471-2105-11-55.
Rahn DD, Ward RM, Sanses TV, Carberry C, Mamik MM, Meriwether KV, et al. Vaginal estrogen use in postmenopausal women with pelvic floor disorders: systematic review and practice guidelines. Int Urogynecol J. 2015;26(1):3–13. https://doi.org/10.1007/s00192-014-2554-z.
Olivera CK, Meriwether K, El-Nashar S, Grimes CL, Chen CC, Orejuela F, et al. Nonantimuscarinic treatment for overactive bladder: a systematic review. Am J Obstet Gynecol. 2016;215(1):34–57. https://doi.org/10.1016/j.ajog.2016.01.156.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. https://doi.org/10.1007/s10654-010-9491-z.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/bmj.d5928.
Wallace BCD, J I, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational Back-end. J Stat Softw. 2012;49(5):5085.
Trikalinos TA, Hoaglin DC, Schmid CH (2013). In: Empirical and Simulation-Based Comparison of Univariate and Multivariate Meta-Analysis for Binary Outcomes. AHRQ Methods for Effective Health Care. Rockville (MD),
Atkins D, Eccles M, Flottorp S, Guyatt GH, Henry D, Hill S, et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches the GRADE working group. BMC Health Serv Res. 2004;4(1):38. https://doi.org/10.1186/1472-6963-4-38.
Kow N, Goldman HB, Ridgeway B. Uterine conservation during prolapse repair: 9-year experience at a single institution. Female Pelvic Med Reconstr Surg. 2016;22(3):126–31. https://doi.org/10.1097/SPV.0000000000000221.
Gutman RE, Rardin CR, Sokol ER, Matthews C, Park AJ, Iglesia CB, et al. Vaginal and laparoscopic mesh hysteropexy for uterovaginal prolapse: a parallel cohort study. Am J Obstet Gynecol. 2017;216(1):38 e31–11. https://doi.org/10.1016/j.ajog.2016.08.035.
Paek J, Lee M, Kim BW, Kwon Y. Robotic or laparoscopic sacrohysteropexy versus open sacrohysteropexy for uterus preservation in pelvic organ prolapse. Int Urogynecol J. 2016;27(4):593–9. https://doi.org/10.1007/s00192-015-2869-4.
Joshi VM, Otiv SR, Dagade VB, Borse M, Majumder RN, Shrivastava M, et al. Pectineal ligament Hysteropexy for uterine prolapse in premenopausal women by open and laparoscopic approach in Indian urban and rural centers. Female Pelvic Med Reconstr Surg. 2015;21(4):215–9. https://doi.org/10.1097/SPV.0000000000000179.
Mourik SL, Martens JE, Aktas M. Uterine preservation in pelvic organ prolapse using robot assisted laparoscopic sacrohysteropexy: quality of life and technique. Eur J Obstet Gynecol Reprod Biol. 2012;165(1):122–7. https://doi.org/10.1016/j.ejogrb.2012.07.025.
Costantini E, Lazzeri M, Zucchi A, Bini V, Mearini L, Porena M. Five-year outcome of uterus sparing surgery for pelvic organ prolapse repair: a single-center experience. Int Urogynecol J. 2011;22(3):287–92. https://doi.org/10.1007/s00192-010-1342-7.
Rahmanou P, White B, Price N, Jackson S. Laparoscopic hysteropexy: 1- to 4-year follow-up of women postoperatively. Int Urogynecol J. 2014;25(1):131–8. https://doi.org/10.1007/s00192-013-2209-5.
Fayyad AM, Siozos CS. Safety and one year outcomes following vaginally assisted laparoscopic uterine sacropexy (VALUES) for advanced uterine prolapse. Neurourol Urodyn. 2014;33(3):345–9. https://doi.org/10.1002/nau.22433.
Grimminck K, Mourik SL, Tjin-Asjoe F, Martens J, Aktas M. Long-term follow-up and quality of life after robot assisted sacrohysteropexy. Eur J Obstet Gynecol Reprod Biol. 2016;206:27–31. https://doi.org/10.1016/j.ejogrb.2016.06.027.
Kupelian AS, Vashisht A, Sambandan N, Cutner A. Laparoscopic wrap round mesh sacrohysteropexy for the management of apical prolapse. Int Urogynecol J. 2016;27(12):1889–97. https://doi.org/10.1007/s00192-016-3054-0.
Khan A, Jaleel R, Nasrullah FD. Sacrohysteropexy performed as uterus conserving surgery for pelvic organ prolapse: review of case files. Pak J Med Sci. 2016;32(5):1174–8. https://doi.org/10.12669/pjms.325.10307.
Krause HG, Goh JT, Sloane K, Higgs P, Carey MP. Laparoscopic sacral suture hysteropexy for uterine prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(4):378–81. https://doi.org/10.1007/s00192-005-0019-0.
Hsieh CH. A new laparoscopic technique for uterine prolapse: one-sided uterine fixation through the round ligament. Int Urogynecol J. 2011;22(2):213–9. https://doi.org/10.1007/s00192-010-1269-z.
Rimailho J, Talbot C, Bernard JD, Hoff J, Becue J. Anterolateral hysteropexy via abdominal approach. Results and indications. Apropos of a series of 92 patients. Ann Chir. 1993;47(3):244–9.
Khanam RA, Rubaiyat A, Azam MS. Sling for correcting uterine prolapse: twelve years experience. Mymensingh Med J. 2014;23(1):13–7.
Veit-Rubin N, Dubuisson JB, Lange S, Eperon I, Dubuisson J. Uterus-preserving laparoscopic lateral suspension with mesh for pelvic organ prolapse: a patient-centred outcome report and video of a continuous series of 245 patients. Int Urogynecol J. 2016;27(3):491–3. https://doi.org/10.1007/s00192-015-2859-6.
Diwan A, Rardin CR, Strohsnitter WC, Weld A, Rosenblatt P, Kohli N. Laparoscopic uterosacral ligament uterine suspension compared with vaginal hysterectomy with vaginal vault suspension for uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(1):79–83. https://doi.org/10.1007/s00192-005-1346-x.
Khandwala S, Williams C, Reeves W, Dai J, Jayachandran C. Role of vaginal mesh hysteropexy for the management of advanced uterovaginal prolapse. J Reprod Med. 2014;59(7–8):371–8.
Sheng Q, Ma N, Huang H, Xu B, He C, Song Y. Significance of preoperative calculation of uterine weight as an indicator for preserving the uterus in pelvic reconstructive surgery. Int J Clin Exp Pathol. 2015;8(1):900–5.
Jirschele K, Seitz M, Zhou Y, Rosenblatt P, Culligan P, Sand P. A multicenter, prospective trial to evaluate mesh-augmented sacrospinous hysteropexy for uterovaginal prolapse. Int Urogynecol J. 2015;26(5):743–8. https://doi.org/10.1007/s00192-014-2564-x.
Khandwala S. Transvaginal mesh surgery for pelvic organ prolapse: one-year outcome analysis. Female Pelvic Med Reconstr Surg. 2013;19(2):84–9. https://doi.org/10.1097/SPV.0b013e31827de6de.
Geoffrion R, Hyakutake MT, Koenig NA, Lee T, Cundiff GW. Bilateral sacrospinous vault fixation with tailored synthetic mesh arms: clinical outcomes at one year. J Obstet Gynaecol Can. 2015;37(2):129–37.
Del Amo E, Burcet G, Vellvé K, Hernández J, Carreras R. Quality of life and patients satisfaction after genital prolapse surgery: vaginal hysterectomy versus mesh hysteropexy. Abstracts of the 44th annual meeting of the international continence society (ICS) 20-24 October, 2014, Rio de Janeiro, Brazil. Neurourol Urodyn. 2014;33(6):631–1071. https://doi.org/10.1002/nau.22655.
de Landsheere L, Ismail S, Lucot JP, Deken V, Foidart JM, Cosson M. Surgical intervention after transvaginal Prolift mesh repair: retrospective single-center study including 524 patients with 3 years’ median follow-up. Am J Obstet Gynecol. 2012;206(1):83 e81–7. https://doi.org/10.1016/j.ajog.2011.07.040.
Malandri M, Iordanidou E, Takou M, Moraitis B, Balaxis D. A randomized comparison of two vaginal procedures for the treatment of stage two, or higher uterine prolapse: hysterectomy with mesh versus only mesh implantation. Neurourol Urodyn. 2012;31(6):855.
Lin TY, Su TH, Wang YL, Lee MY, Hsieh CH, Wang KG, et al. Risk factors for failure of transvaginal sacrospinous uterine suspension in the treatment of uterovaginal prolapse. J Formos Med Assoc. 2005;104(4):249–53.
Dietz V, Huisman M, de Jong JM, Heintz PM, van der Vaart CH. Functional outcome after sacrospinous hysteropexy for uterine descensus. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):747–52. https://doi.org/10.1007/s00192-007-0520-8.
Dietz V, de Jong J, Huisman M, Schraffordt Koops S, Heintz P, van der Vaart H. The effectiveness of the sacrospinous hysteropexy for the primary treatment of uterovaginal prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(11):1271–6. https://doi.org/10.1007/s00192-007-0336-6.
Dubernard G, Rouzier R, Haddad B, Dubois P, Paniel BJ. Correction of uterine prolapse by the vaginal route using the uterosacral ligaments: Shirodkar procedure. Eur J Obstet Gynecol Reprod Biol. 2003;109(2):214–8.
Bohoussou E, Adjoussou SA, Letouzey V, Fatton B, de Tayrac R. Should we perform intra-operative endometrial biopsy during pelvic reconstructive surgery with uterine preservation? J Gynecol Obstet Biol Reprod (Paris). 2014;43(1):40–5. https://doi.org/10.1016/j.jgyn.2013.10.011.
Abdulsid ATG, Jani M, Elsapagh K, Allam M. Sacrospinous fixation, keep or remove the uterus? That is the question Gynecol Surg. 2016;13(Suppl 1):S1–S453.
Romanzi LJ, Tyagi R. Hysteropexy compared to hysterectomy for uterine prolapse surgery: does durability differ? Int Urogynecol J. 2012;23(5):625–31. https://doi.org/10.1007/s00192-011-1635-5.
Farthmann J, Watermann D, Erbes T, Roth K, Nanovska P, Gitsch G, et al. Functional outcome after pelvic floor reconstructive surgery with or without concomitant hysterectomy. Arch Gynecol Obstet. 2015;291(3):573–7. https://doi.org/10.1007/s00404-014-3435-x.
Nava y Sanchez RM, Acosta RU, Ruiz Velasco V, Garcia TL. Manchester’s operation. I. Morbimortality and early complications. Ginecol Obstet Mex. 1973;33(198):347–60.
Oversand SH, Staff AC, Spydslaug AE, Svenningsen R, Borstad E. Long-term follow-up after native tissue repair for pelvic organ prolapse. Int Urogynecol J. 2014;25(1):81–9. https://doi.org/10.1007/s00192-013-2166-z.
Ayhan A, Esin S, Guven S, Salman C, Ozyuncu O. The Manchester operation for uterine prolapse. Int J Gynaecol Obstet. 2006;92(3):228–33. https://doi.org/10.1016/j.ijgo.2005.12.002.
Conger GT, Keettel WC. The Manchester-fothergill operation, its place in gynecology; a review of 960 cases at university hospitals, Iowa City. Iowa Am J Obstet Gynecol. 1958;76(3):634–40.
Tipton RH, Atkin PF. Uterine disease after the Manchester repair operation. J Obstet Gynaecol Br Commonw. 1970;77(9):852–3.
Carey MP, Slack MC. Transvaginal sacrospinous colpopexy for vault and marked uterovaginal prolapse. Br J Obstet Gynaecol. 1994;101(6):536–40.
Lo TS, Pue LB, Hung TH, Wu PY, Tan YL. Long-term outcome of native tissue reconstructive vaginal surgery for advanced pelvic organ prolapse at 86 months: hysterectomy versus hysteropexy. J Obstet Gynaecol Res. 2015;41(7):1099–107. https://doi.org/10.1111/jog.12678.
Dietz V, CH vV, APM H, SE S-K. Vaginal hysterectomy versus sacrospinous hysteropexy as primary treatment of prolapse: a randomized controlled trial (RCT), a preliminary report (abstract number 285). Int Urogynecol J. 2006;17(Suppl. 2):S171–359.
Jeng CJ, Yang YC, Tzeng CR, Shen J, Wang LR. Sexual functioning after vaginal hysterectomy or transvaginal sacrospinous uterine suspension for uterine prolapse: a comparison. J Reprod Med. 2005;50(9):669–74.
van Brummen HJ, van de Pol G, Aalders CI, Heintz AP, van der Vaart CH. Sacrospinous hysteropexy compared to vaginal hysterectomy as primary surgical treatment for a descensus uteri: effects on urinary symptoms. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(5):350–355; discussion 355. https://doi.org/10.1007/s00192-003-1084-x.
Kalogirou D, Antoniou G, Karakitsos P, Kalogirou O. Comparison of surgical and postoperative complications of vaginal hysterectomy and Manchester procedure. Eur J Gynaecol Oncol. 1996;17(4):278–80.
Catanzarite T, Rambachan A, Mueller MG, Pilecki MA, Kim JY, Kenton K. Risk factors for 30-day perioperative complications after Le fort colpocleisis. J Urol. 2014;192(3):788–92. https://doi.org/10.1016/j.juro.2014.03.040.
Ubachs JM, van Sante TJ, Schellekens LA. Partial colpocleisis by a modification of LeFort’s operation. Obstet Gynecol. 1973;42(3):415–20.
Mueller MG, Ellimootil C, Abernethy MG, Mueller ER, Hohmann S, Kenton K. Colpocleisis: a safe, minimally invasive option for pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2015;21(1):30–3. https://doi.org/10.1097/SPV.0000000000000114.
Szczesniewska A, Szpakowski M, Wladzinski J, Wilczynski JR. (un)forgotten Neugebauer-Le fort operation. Paramedian closure of the vagina--safe and effective surgical procedure for treating of pelvic organ prolapse in older women. Ginekol Pol. 2015;86(3):198–202.
Marin Ardila L. Le Fort’s colpocleisis. 10-year study in the gynecology and obstetrics Department of the Hospital san Juan de Dios in Bogota. Rev Colomb Obstet Ginecol. 1966;17(6):415–24.
Goldman J, Ovadia J, Feldberg D. The Neugebauer-Le fort operation: a review of 118 partial colpocleises. Eur J Obstet Gynecol Reprod Biol. 1981;12(1):31–5.
Falk HC, Kaufman SA. Partial colpocleisis: the Le fort procedure; analysis of 100 cases. Obstet Gynecol. 1955;5(5):617–27.
Wang X, Chen Y, Hua K. Pelvic symptoms, body image, and regret after LeFort Colpocleisis: a long-term follow-up. J Minim Invasive Gynecol. 2017;24(3):415–9. https://doi.org/10.1016/j.jmig.2016.12.015.
Denehy TR, Choe JY, Gregori CA, Breen JL. Modified Le fort partial colpocleisis with Kelly urethral plication and posterior colpoperineoplasty in the medically compromised elderly: a comparison with vaginal hysterectomy, anterior colporrhaphy, and posterior colpoperineoplasty. Am J Obstet Gynecol. 1995;173(6):1697–701 discussion 1701-1692.
Geynisman-Tan J, Kenton K. Surgical updates in the treatment of pelvic organ prolapse. Rambam Maimonides Med J. 2017;8(2). https://doi.org/10.5041/RMMJ.10294.
Younger A, Rac G, Clemens JQ, Kobashi K, Khan A, Nitti V, et al. Pelvic organ prolapse surgery in academic female pelvic medicine and reconstructive surgery urology practice in the setting of the Food and Drug Administration public health notifications. Urology. 2016;91:46–51. https://doi.org/10.1016/j.urology.2015.12.057.
Elterman DS, Chughtai BI, Vertosick E, Maschino A, Eastham JA, Sandhu JS. Changes in pelvic organ prolapse surgery in the last decade among United States urologists. J Urol. 2014;191(4):1022–7. https://doi.org/10.1016/j.juro.2013.10.076.
Aarts JW, Nieboer TE, Johnson N, Tavender E, Garry R, Mol BW, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2015;8:CD003677. https://doi.org/10.1002/14651858.CD003677.pub5.
Committee on Gynecologic P. Committee opinion no 701: choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2017;129(6):e155–9. https://doi.org/10.1097/AOG.0000000000002112.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. 2016;10:CD012376. https://doi.org/10.1002/14651858.CD012376.
Practice Bulletin No. 176 Summary: Pelvic Organ Prolapse. Obstet Gynecol. 2017;129(4):763–5. https://doi.org/10.1097/AOG.0000000000002008.
FitzGerald MP, Richter HE, Siddique S, Thompson P, Zyczynski H, Ann Weber for the Pelvic Floor Disorders N. Colpocleisis: a review. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(3):261–71. https://doi.org/10.1007/s00192-005-1339-9.
De Vita D, Araco F, Gravante G, Sesti F, Piccione E. Vaginal reconstructive surgery for severe pelvic organ prolapses: a ‘uterine-sparing’ technique using polypropylene prostheses. Eur J Obstet Gynecol Reprod Biol. 2008;139(2):245–51. https://doi.org/10.1016/j.ejogrb.2008.01.013.
Huang KH, Chuang FC, Fu HC, Kung FT. Polypropylene mesh as an alternative option for uterine preservation in pelvic reconstruction in patients with uterine prolapse. J Obstet Gynaecol Res. 2012;38(1):97–101. https://doi.org/10.1111/j.1447-0756.2011.01647.x.
Milani AL, Withagen MI, Vierhout ME. Outcomes and predictors of failure of trocar-guided vaginal mesh surgery for pelvic organ prolapse. Am J Obstet Gynecol. 2012;206(5):440 e441–8. https://doi.org/10.1016/j.ajog.2012.01.039.
Meschia M, Pifarotti P, Bernasconi F, Magatti F, Riva D, Kocjancic E. Porcine skin collagen implants to prevent anterior vaginal wall prolapse recurrence: a multicenter, randomized study. J Urol. 2007;177(1):192–5. https://doi.org/10.1016/j.juro.2006.08.100.
Feiner B, Gietelink L, Maher C. Anterior vaginal mesh sacrospinous hysteropexy and posterior fascial plication for anterior compartment dominated uterovaginal prolapse. Int Urogynecol J. 2010;21(2):203–8. https://doi.org/10.1007/s00192-009-1012-9.
Fink K, Shachar IB, Braun NM. Uterine preservation for advanced pelvic organ prolapse repair: anatomical results and patient satisfaction. Int Braz J Urol. 2016;42(4):773–8. https://doi.org/10.1590/S1677-5538.IBJU.2015.0656.
Li BH, Huang HJ, Song YF. Modified Prolift procedure without trachelectomy or hysterectomy for the treatment of advanced pelvic organ prolapse complicated with cervical elongation. Zhonghua Fu Chan Ke Za Zhi. 2016;51(3):174–9. https://doi.org/10.3760/cma.j.issn.0529-567X.2016.03.003.
Acknowledgments
This work is supported by the Society of Gynecologic Surgeons (SGS), whose members comprise the Systematic Review Group (SRG) performing this review. SGS supports the SRG with provision of meeting space and oversight, and aids in the public dissemination of study findings to its members. SGS funds Dr. Balk as a paid methodological consultant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
KVM is a textbook editor for Elsevier publications and has not yet received any royalties for that publication. The other authors have no conflicts to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Study Registration
Registration with PROSPERO (CRD42017067899) and full protocol can be found at: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017067899
Paper Presentation Information
Society of Gynecologic Surgeons Annual Scientific Meeting, San Antonio, TX, USA, 26–29 March 2017
Appendix 1: literature search strategy
Appendix 1: literature search strategy
Among the Medical Subject Headings (MeSH) searched were uterine prolapse, pelvic organ prolapse, prolapse, descensus, vaginal prolapse, pelvic floor, rectocele, cystocele, sacrocolpopexy, sacropexy, colpopexy, hysteropexy, uterine preservation, Manchester, colpocleisis, Fothergill, LeFort, randomized trial, longitudinal studies, clinical trial, controlled clinical trial, comparative study, prospective study, retrospective study, meta-analysis, and systematic review. Included studies could be in any published format (e.g., journal article, abstract, poster) as long as data could be extracted from the form in which it was published. We did not attempt to identify unpublished articles or abstracts, and we did not contact study authors. The search was limited to humans and included any language. Studies in languages that were not fluently read by one of our group members were interpreted with the assistance of a fluent speaker in the medical field or with professional translational software to extract relevant findings. Reference lists of selected articles and review papers were screened for additional eligible references.
Rights and permissions
About this article
Cite this article
Meriwether, K.V., Balk, E.M., Antosh, D.D. et al. Uterine-preserving surgeries for the repair of pelvic organ prolapse: a systematic review with meta-analysis and clinical practice guidelines. Int Urogynecol J 30, 505–522 (2019). https://doi.org/10.1007/s00192-019-03876-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03876-2